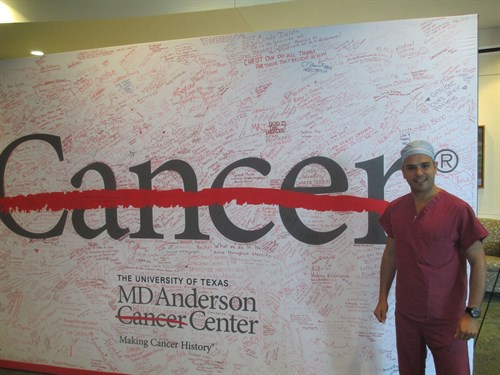
Daniel Leff's Ronald Raven Travelling Fellowship 2013
A report on a combined surgical oncology and plastic surgical two-week observership at the MD Anderson Cancer Centre in Houston, Texas
I was privileged to receive one of the BASO Ronald Raven
Travelling Fellowships awarded in 2013 and used the funding towards
a combined surgical oncology and plastic surgical two-week
observership at the MD Anderson Cancer Centre in Houston, Texas
("Oncoplastics" doesn't exist in the USA and my advice is it's
probably best not to mention it!).
MD Anderson is one of the world's premier cancer centres, treating
nearly 120,000 patients and performing 66,000 surgeries hours per
year. MD Anderson is located within the Texas Medical Centre,
which employs over 106,000 people (more than Apple and Google) of
which 1 in 5 are employed in the health science field, making it
the largest concentration of life science professionals anywhere in
the world. As soon as you arrive at MD Anderson you are
struck by its sheer scale and enormity. The three primary
buildings: "Main", "Faculty" and "Mays" are connected by vast sky
bridges suspended over the freeways. Walking down these will
certainly keep you fit but there is always the option of taking the
golf buggy that transports patients and relatives (but only if
there is room on the back!). The hospital has an aquarium, an art
gallery and a 'park', and the sounds of the piano and flute can
regularly be heard down the hallways (yes, you read all that
correctly…just like any old UK NHS Trust!).
I was lucky to be supervised throughout my stay by Professor Henry
Mark Kuerer who is as charming, bright and quick-witted as he is
reserved and unassuming. He made me feel part of the team
immediately and was happy to be quizzed incessantly on his
rationale for almost every decision he was making. The cases were
complex in the extreme. Ductal carcinoma in situ treated by
mastectomy with positive anterior and posterior margins… what would
you do, he asked? (Nothing especially inspiring from me!). Prof
Kuerer calmly gave the patients all the options from further skin
excision to hormone therapy only and radiotherapy. A patient
with sporadic, node-positive, inflammatory breast cancer requested
contralateral mastectomy. "Approximately 30-40% of patients request
contralateral mastectomy here," Prof Kuerer informed me.
Quite staggering. He advised her to treat the primary
disease and delay decision-making regarding the contralateral
breast. A patient with history of mantle radiotherapy who is
undergoing MRI surveillance has been found to have lobular
carcinoma in situ and atypical ductal hyperplasia. Prof
Kuerer attends the patient with a clinician with a specialist
interest in "Cancer Prevention" (… a branch of medicine I suspect
yet to be established in the UK). The discussion includes the
option for surgery but was also heavily focused on the benefits and
side effects of Tamoxifen to reduce the risk of breast cancer in
women at high risk. Despite NICE guidance on the benefits of
Tamoxifen, I had yet to experience a clinician offer Tamoxifen as a
preventative strategy to women in the UK. Finally, a patient
arrives with a second episode of locally-recurrent disease having
previously had breast conserving surgery and radiotherapy twice
(…twice I thought…isn't that illegal!). It turns out she opted for
a clinical trial of breast conserving surgery and partial breast
radiotherapy when she recurred the first time. "Won't recommend
that again," Prof Kuerer shrugs, and we go to lunch.
I had the pleasure of observing Sarah DeSynder operate. 07.30am
(…yes 07.30am sharp!) WHO-style checklist performed in the
operating theatre with the whole team present and whilst the
patient was still awake. (There are no anaesthetic rooms). Gave the
patient the chance to tell them not to operate on the left breast
(the consent clearly spelt out bilateral breast surgery!).
There was a lot of innovation to see. A patient was having
radio-labelled seed guided excision of an area of ductal carcinoma
in situ. Seed localised surgery is actually more intuitive
than I had appreciated, and it avoids many of the problems of
needle localisation. Abnormal axillary lymph nodes are
clipped at diagnosis and radiolabelled seeds are subsequently
placed to see the effects following neoadjuvant chemotherapy and to
determine how often the clipped node is indeed the sentinel node.
Smart study. Specimens were taken to the pathology department by Dr
DeSnyder herself (pathology being co-located and just opposite
theatres) and the chief breast pathologist showed me how they ink
and cut the specimens. They also take specimen radiographs and use
themto try to gauge the chances of margin positivity in real time.
DeSnyder, the pathologist and the radiologist had a mini-MDT over
one of the cases prompting her to take a further inferior margin.
How fabulous is that. I would typically have to wait 10 days
to decide whether or not to re-operate for close or positive
margins.
I observed one of the plastic surgeons, Dr Melissa Crosby,
performing an implant exchange and a delayed latissimus dorsi flap
reconstruction. She was full of great advice. She
taught me her technique for dropping and re-anchoring the
infra-mammary fold, explained the benefits of being able to sit the
patients up repeatedly to check reconstructive symmetry, emphasised
the value of on-table expandable sizers before determining the
definitive implant, and explained the use of round implants to
create…. in her words that "barbie-doll look"! Oh, and always
use "holy water" (….a term I later found out means saline and
antibiotics mix) in the implant pocket.
Another plastic surgeon, Dr Alderman, took time out to show images
depicting some of the more extreme effects of radiotherapy
delivered at MD Anderson. We discussed the impact of the regimens
used on reconstruction. Patients in need of PMRT tend not to be
offered an immediate free flap reconstruction at MD Anderson and
they opt instead for the delayed-immediate technique. Then I
observed Dr Mark Villa perform a therapeutic mammoplasty using a
vertical scar inferior pedicle technique and used the opportunity
to discuss and revise different skin patterns and pedicles with
him. Finally, I was able to network with Professor Oliver Bogler,
one of the leaders of the global academic programme (GAP), and had
an opportunity to brainstorm ideas for collaboration and joint
grant funding.
However, of all the things I observed, it is the MD Anderson
approach to clinical care and treatment of staff that most stands
out. They really celebrate survivorship! (…how very American you
may say!). If you survive cancer they make a very big deal of it,
and in my view it should be and we could all learn from that. You
can't walk down a hallway or enter a clinic without seeing a banner
or a plaque that describes someone's struggle through adversity.
They are fully focused on patient experience and there are several
picturesque places throughout the hospital to take solace, learn
and read (there are several learning centres specific for patients)
or simply to talk to other cancer sufferers about their
experiences. The most remarkable centre for children, called
"Kim's place" (named after Kim Perrot, a famous basketball player
who contracted cancer) is filled with basket-ball hoops, pool
tables, video-games, and a full sized cinema screen and it allows
paediatric patients to taste a degree of normality. From my
experience, patients really appreciate all this effort and they are
willing to travel thousands of miles across the USA to be treated
at MD Anderson. Staff are celebrated similarly. There are
plaques celebrating divisional employee of the month on all the
walls throughout the hospital. I witnessed the new medical
director address the entire theatre staff, and explain the culture
of openness he wanted to foster: "If you have a problem with me…
come to me and I will do the same for you. If someone comes to you
and they have a problem with me, tell them to come to me. If
you and someone else have a problem with me …say let's go see him
together!"... Inspirational stuff.
My stay was made so much more enjoyable and productive for meeting
two very special clinicians: Professor Alastair Thompson (the then
Breast CSG chair) a breast surgeon oncologist who arrived at MD
Anderson via Dundee, and his wife Stacey Moulder, a clinical
oncologist. They explained the fundamentals of how MD Anderson
functions (both good and bad), facilitated observation in theatre
and outpatient clinics, took me along to combined MDTs, helped me
find my around and were thoroughly generous with their time outside
of work. Houston isn't an especially top tourist destination
I was told, but I was very thankful nevertheless to be pointed in
the direction of RICE university district, the Minute Maid Baseball
Stadium, and Hermann Park, all of which served up a treat.
I leave you with a mantra I saw typed on one of the Professor's
doors at MD Anderson and that I am trying to take back into my
clinical practice: "Treat the disease and you may win or lose.
Treat the patient and you win, no matter the outcome".
Daniel Leff